Total Hip Replacement
What is Normal Hip Anatomy?
The hip is one of the body's largest weight-bearing joints. It consists of two main parts: a ball (femoral head) at the top of your thighbone (femur) that fits into a rounded socket (acetabulum) in your pelvis. Bands of tissue called ligaments (hip capsule) connect the ball to the socket and provide stability to the joint. The bony surfaces of the ball and socket have a smooth durable cover of articular cartilage that cushions the ends of the bones and enables them to move easily. A thin, smooth tissue called synovial membrane covers all remaining surfaces of the hip joint. In a healthy hip, this membrane makes a small amount of fluid that lubricates and almost eliminates friction in your hip joint. Normally, all the parts of your hip work in harmony, allowing you to move easily and without pain.
Common reasons for Total Hip Arthroplasty
The most common cause of chronic hip pain and disability is arthritis. Osteoarthritis, rheumatoid arthritis, avascular necrosis and traumatic arthritis are the most common forms of this disease. Most people who undergo hip replacement surgery experience a dramatic reduction of hip pain and a significant improvement in their ability to perform the common activities of daily living. While some patients can return to higher levels of activity, most patients are not able to return to high-impact sports or running.
What does a Total Hip Replacement procedure involve?
The operation is performed under general or spinal anaesthesia and typically takes 1–2 hours.
Your surgeon will:
Make an incision along the side or front of the hip, depending on the approach used.
Carefully remove the damaged cartilage and bone from both the femoral head and acetabulum.
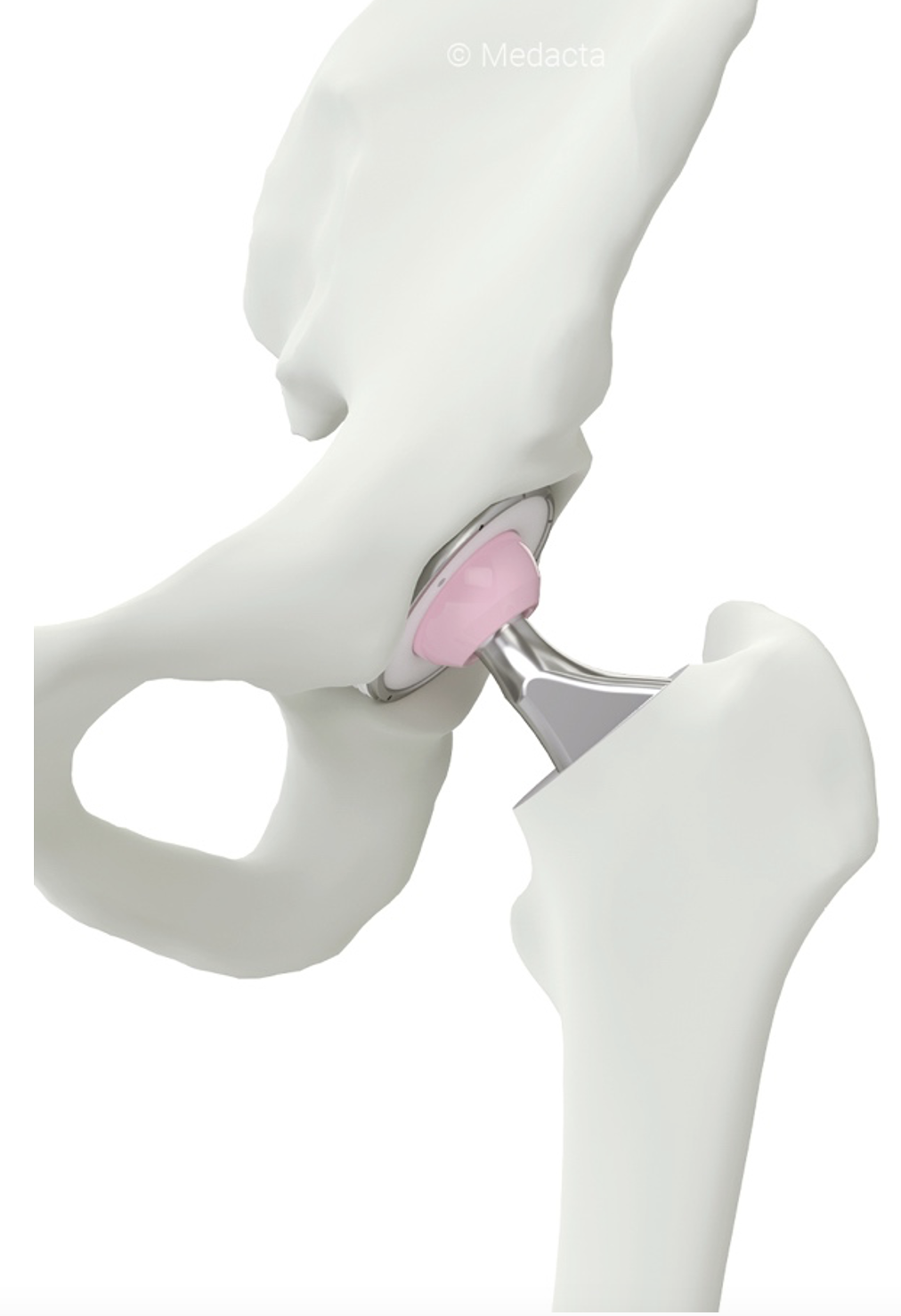
Prepare the pelvic socket (acetabulum) and place a new cup component made of metal, plastic, or ceramic.
Shape the femoral canal inside the thigh bone and insert a stem component that supports the new ball.
Fit the ball into the socket liner, ensuring smooth movement and stability which are made of either metal, ceramic, or plastic.
All components are secured either by press-fit fixation (allowing bone to grow onto the implant) or with surgical cement depending on bone quality, patient factors and surgeon preference. The incision is then closed, and sterile dressings are applied. Most patients begin walking with assistance on the same or the next day.
What is the difference between a Posterior vs Anterior Hip Replacement?
The posterior and anterior approaches describe how the surgeon accesses the hip joint, not the type of implant used. Both approaches can produce excellent long-term results, and your surgeon will recommend the most appropriate one based on your anatomy, lifestyle, and specific needs.
Posterior Approach
Incision location: Made at the back (posterior) of the hip.
Muscles affected: Small external rotator muscles are detached and later repaired.
Advantages:
Excellent exposure for complex anatomy or revisions
Widely used and well-studied with proven long-term outcomes
Easier access for implant positioning
Considerations:
Slightly higher early risk of dislocation (minimized with modern techniques)
Early recovery can be more painful
Anterior Approach
Incision location: Made at the front (anterior) of the hip.
Muscles affected: Performed between muscles rather than detaching them (“muscle-sparing”).
Advantages:
Smaller incisions and potentially less early muscle damage
Faster initial recovery and low early dislocation risk
Considerations:
Technically more demanding; not suitable for all patients (especially very muscular or obese individuals)
Possible temporary/permanent numbness from stretching of small nerves near the incision
No proven long-term functional difference compared with the posterior approach
In summary: Both techniques aim to achieve the same outcome — a stable, pain-free, well-aligned hip. Your surgeon will discuss which approach best fits your condition and anatomy.
More details about Total Hip Replacement
How do I prepare for surgery?
Medical Evaluation: In preparation for surgery, you may be asked to have a complete physical examination by our referring medical physician before your surgery. This is needed to assess your health and identify conditions that can interfere with your surgery or recovery. Additional approval for surgery may be needed if you also receive medical care from a specialist such as a cardiologist or a urologist.
Tests: Several tests may be needed to help plan your surgery: blood and urine samples may be tested, and an electrocardiogram and chest x-rays may be ordered.
Medications: Ensure that all medical providers are aware of what medications you are taking. At your medical evaluation you will be informed which medications you should continue or stop taking before surgery. Some unique medications may require your specialist’s input as to when to stop or continue taking.
Imaging: In preparation for surgery, additional imaging, such as a CT scans and X-rays may be ordered to plan for implant placement and size.
What to expect from my recovery
Short-Term Recovery (First 6–12 Weeks)
Hospital stay: Usually 1–3 days. You will begin walking with a physiotherapist soon after surgery.
Pain and swelling: Common in the first few weeks; managed with medication, ice, and rest. The anesthetist will discuss the possibility of placing a spinal block during the procedure, which will help with pain during your first day of recovery. You will be given pain medication which have side effects such as nausea, vomiting, and dependency.
Mobility: You’ll use crutches or a walker for support for approximately 2–6 weeks.
Physiotherapy: Focuses on gentle range of motion, walking, and early strengthening.
Daily activities: Most patients can perform light household tasks by 3–4 weeks
Most people who undergo hip replacement surgery experience a dramatic reduction of hip pain and a significant improvement in their ability to perform the common activities of daily living. While some patients can return to higher levels of activity, most patients are not able to return to high-impact sports or running.
How do I manage my wound?
Dressings: Keep your waterproof dressing on for 2 weeks. You will need to have a wound check with your GP at the 2-week mark.
Showering: You may shower with the waterproof dressing on. Avoid soaking the wound (no baths, pools, or spas) until 6 weeks.
Inspection: Check the incision daily for infection, such as redness, foul-smelling drainage, or unusual pain. Fevers also occur when the wound in infected. Please contact our clinic if you experience any of these symptoms.
Sutures: Dissolvable sutures are used for closure and do not require removal. Some of the sutures do not dissolve and will be pushed out by your skin naturally.
Clothing: Avoid tight clothing or pressure over the incision to prevent irritation.
When can I return to work after a hip replacement?
Returning to work depends on the nature of your occupation. If you have a sedentary office job you can expect to return to work in 1-2 weeks. A heavy duty occupation can take 2-3 months to return to a full compacity.
When can I go back to driving?
For a left hip replacement, one can return to driving an automatic transmition vehicle in 1-2 weeks. A right hip replacement will require more time to return to driving and typically takes 8-10 weeks.
Surgical Risks & Possible Complications
1. Infection
Can occur around the wound or deep in the joint/implant.
Prevented with antibiotics and sterile surgical techniques.
Deep infections may require further surgery such as removal of implants, revision hip arthroplasty, and prolong course of antibiotics.
2. Blood Clots (Deep Vein Thrombosis / Pulmonary Embolism)
Clots can form in the leg veins after surgery and travel to the lungs which can be life-threatening.
Prevented with early mobilisation, compression stockings, and blood-thinning medication (aspirin/clexane).
3. Dislocation
The artificial ball can come out of the socket, particularly in the early weeks after surgery.
Some patients are at higher risk of this occurring (alcohol abuse, ANV)
This can also occur if the implants are not placed in an obtimal position
4. Leg Length Difference (LLD)
Slight variations in leg length can occur (< 2 cm); this is often minor and correctable with a shoe insert if symptomatic.
It is important to note that a hip replacement cannot correct a LLD that is derived from the knee, leg, or ankle.
Often a patient will feel as if they have a LLD after surgery, even though the implants are appropriately placed and the limbs are effectively equal. This will improve over time with rehabilitation.
A LLD can occur in cases where there is a previous hip deformity or the implants will not be stable unless the limb is lengthened.
5. Fracture
Rarely, the bones around the implant can crack during or after surgery, requiring fixation or revision.
6. Nerve or Blood Vessel Injury
Temporary numbness or weakness can occur due to nerve stretch or bruising.
Permanent injury is extremely rare but it can occur
7. Loosening, Wear, or Gross Failure of the Implant
Over many years, wear and loosening can occur, leading to pain or reduced function.
Gross failure can occur unexpectedly from trauma or implant design and/or manufacturing.
May require revision surgery in the long term.
8. Persistent Pain or Stiffness
Some patients may continue to experience discomfort or limited range of motion despite successful surgery.
9. Heterotopic Ossification
Abnormal bone formation around the joint can cause stiffness; prevented with specific medications or radiation in high-risk cases.
10 Bleeding/hematoma
Blood loss occurs after all surgeries and there is a moderate amount of bleeding after a hip replacement. This may require a blood transfusion after surgery.
Hematomas may cause swelling and pain in the thigh and groin. Most of these resolve over time and do not require treatment. There are situations where they are required to be washed out in theatre but this is a rarity.
11 Risk of Anesthetic
Risk of heart attack, stroke, respiratory failure, kidney failure, and other medical complications including death (which is very rare)