Hip Arthroscopy
What is Hip Arthroscopy?
Hip arthroscopy is a minimally invasive procedure that allows direct visualization of the hip joint for both diagnosis and treatment. It is commonly performed to address:
Labral tears
Cartilage injuries
Impinging CAM lesions of the femur
Iliopsoas snapping
Ruptured ligamentum teres
Loose bodies
How is Hip Arthroscopy performed?
The procedure is performed under sterile conditions in the operating room. You will be positioned either supine or on your side. Gentle traction is applied to your leg to create space within the joint. Careful padding is placed to protect pressure points and maintain comfort.
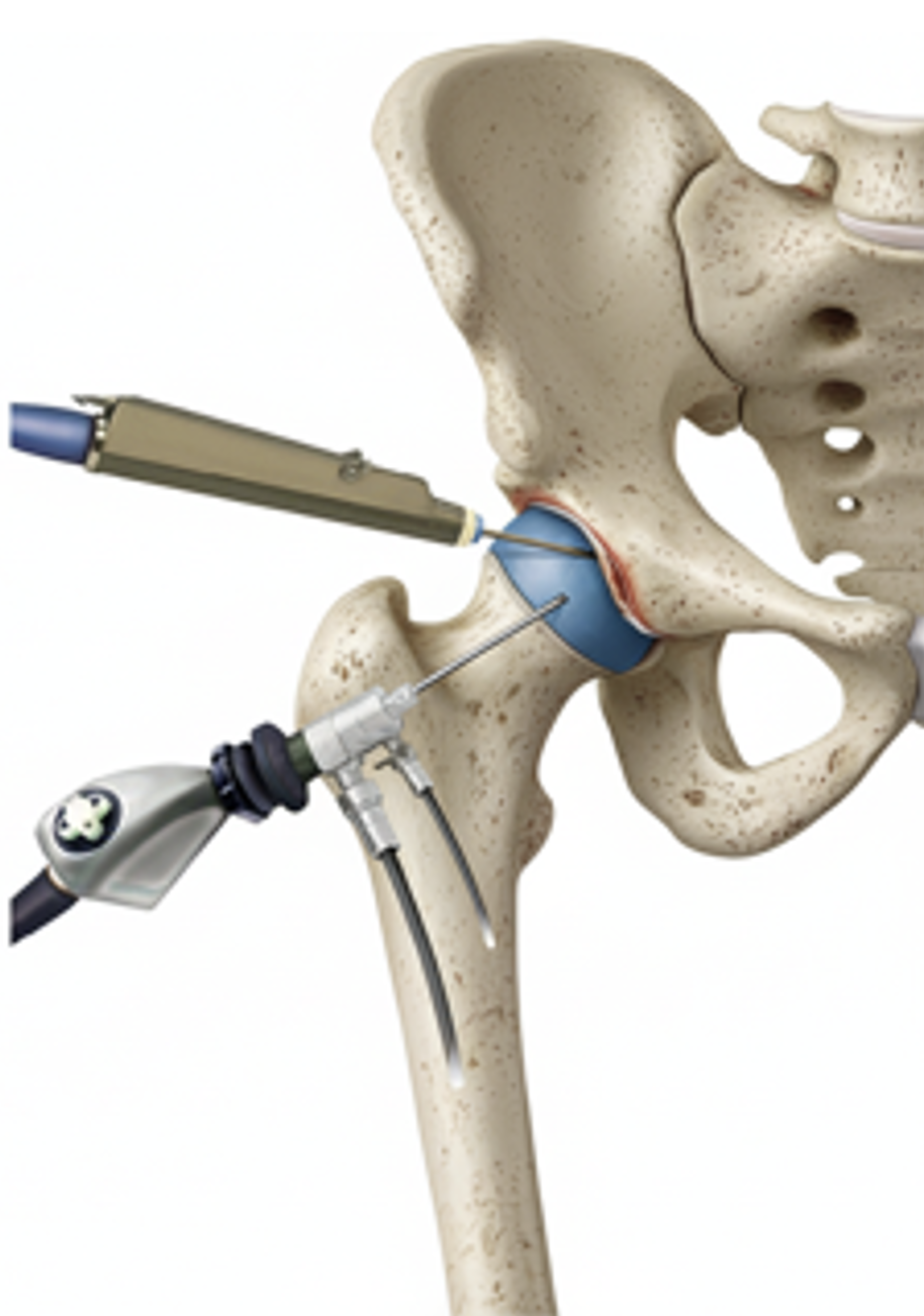
A small incision is made near the hip to access the joint. Fluid is introduced to expand the space, and a camera (arthroscope) with a light source is inserted. Specialized instruments are then used to treat the affected structures.
At the end of the procedure, the small incisions are closed with sutures and covered with a sterile dressing.
What are the advantages of Arthroscopy?
Historically, most hip-preserving procedures required open surgical hip dislocation, which involved large incisions and longer recovery times. Hip arthroscopy, developed in the early 2000s, offers a less invasive alternative. Because hip arthroscopy is a technically demanding procedure, it should be performed by an experienced surgeon.
Advantages over open surgery include:
Smaller incisions
Shorter recovery time
Less postoperative pain
Same-day or next-day discharge
Reduced need for pain medication
Less soft tissue damage
What is the recovery in the immediate Postoperative period?
Most patients are discharged on the same day or after an overnight hospital stay. If admitted, a physiotherapist will work with you before discharge. Some patients may require a slightly longer stay depending on their surgery and recovery.
You will usually be weight-bearing as tolerated with crutches for 2–4 weeks. Crutches should be used until pain is minimal and you can walk normally without a limp.
Movement restrictions:
Most cases will require avoidance of external rotation (e.g., crossing your legs or sleeping on your stomach) for 6 weeks.
Avoid prolonged upright sitting for 2–3 weeks to minimize hip irritation.
Return to activity:
Light cycling on a stationary bike can begin as soon as you are home. Start with a high saddle, no resistance, and 20 minutes, 1–2 times per day. Gradually lower the saddle and increase resistance as comfort allows.
Continue daily cycling for 6–12 weeks to maintain mobility and strength.
Running typically resumes around 3–4 months, once pain, swelling, and range of motion have normalized.
Ice therapy: Apply ice three times daily for 7–10 days to reduce pain and swelling. A cooling or continuous passive motion (CPM) machine may be used but is not essential.
How is the wound managed?
It is normal for the top dressing to become moist with arthroscopic fluid in the first 1–2 days.
After 1-2 days, remove the outer dressing and leave the smaller waterproof dressings in place.
Dressings may be removed completely after 7 days.
Incisions typically heal within two weeks.
Showers are permitted after two weeks; cover the wounds with waterproof dressings if showering earlier.
Do not submerge incisions in water (baths, pools, ocean) for 4–6 weeks.
A wound check with your GP at the two-week mark is recommended.
Absorbable sutures are typically used and do not require removal, though occasionally small remnants may naturally surface during healing.
How do I prevent blood clots (DVT/PE)?
Take Aspirin 100 mg twice daily for two weeks (unless you are already on a blood thinner).
Perform ankle flexion and pumping exercises regularly throughout the day.
Wear TED compression stockings on both legs for the first two weeks.
How do I Manage my Pain After Surgery?
Pain levels vary among patients. You will receive pain medication as needed. Be aware that these medications can cause constipation, drowsiness, and dependence. Your anesthetist may use a spinal or regional nerve block to reduce early postoperative pain.
How do I Prevent Heterotopic Ossification?
Naproxen will also be prescribed to reduce the risk of heterotopic ossification (extra bone formation). Inform your doctor if you have any contraindications, such as bleeding disorders, stomach ulcers, inflammatory bowel disease, or kidney problems.
What Issues Should I Call the Clinic?
Call your clinic if you experience:
Severe or persistent pain
Inability to move your hip or leg
Fever or foul-smelling wound drainage
Excessive thigh/calf cramping, pain, or swelling
Bowel or bladder issues
Falls or new injury
Numbness around the genitals or leg
When Can I Drive?
You must not drive while using crutches or taking narcotic medication. Most patients resume driving after 3–6 weeks, once they can safely operate both legs. For left hip surgery in an automatic car, driving may resume in 1-2 weeks.
Should I See a Physiotherapy?
Ongoing physiotherapist supervision is strongly encouraged for an efficient recovery. Our clinic can recommend trusted physiotherapists upon request.
When Can I Return to Work?
This depends on your surgery and job requirements.
Expect to use crutches for 2–4 weeks.
Sedentary workers may return earlier, while those performing heavy labor or driving may require longer before returning to full duties.
Possible RiskComplications
Although complications are rare, patients should be aware of potential risks, including:
Bleeding
Infection
Nerve or blood vessel injury (including femoral or lateral femoral cutaneous nerves, or sensory nerves to the genital area)
Fluid build-up leading to compartment syndrome in the leg or abdomen
Anesthetic complications (rare, including death)
Loss of limb or limb function
Blood clots or pulmonary embolism
Heterotopic ossification (extra bone formation)
Sexual dysfunction
Fracture
Hip stiffness
Persistent pain or failure to improve
Progression of osteoarthritis
Hip dislocation or instability
Avascular necrosis
When Can I Return to Normal Activities?
Every patient’s recovery is unique. Most regain full function and symptom resolution within 6–9 months, though full recovery can take up to one year depending on the surgery and activity level.
Everyday activities: typically resume within 3–6 months.
Recreational athletes: usually return to sport by 6 months.
High-level or professional athletes: may require 9–12 months before full return to play.
Your rehabilitation will progress in structured phases under physiotherapist guidance.