Posterior Cruciate Ligament (PCL) Reconstruction
How Is a PCL Reconstruction Performed?
A PCL reconstruction is performed to restore stability to the knee after the posterior cruciate ligament has been torn or stretched beyond healing capacity. The operation is usually performed arthroscopically (keyhole surgery) under general anesthesia. There are rare situations where open surgery is a preferred technique.
During the procedure:
Small incisions are made to insert a camera and instruments into the knee.
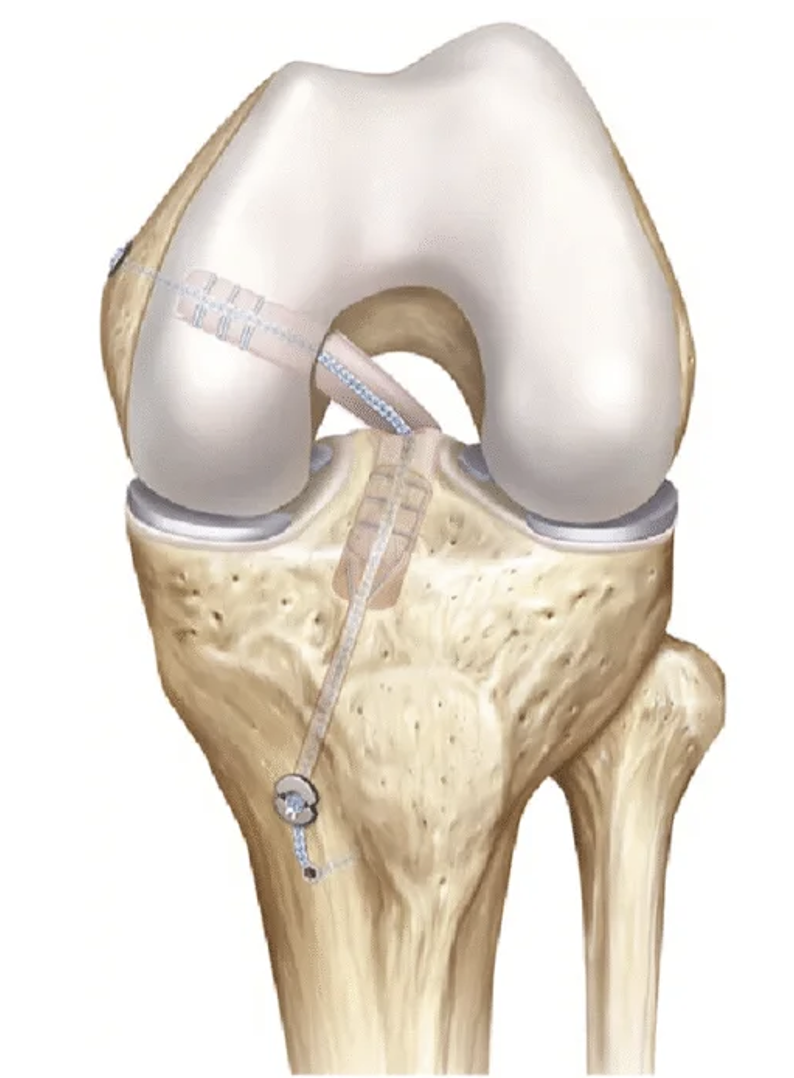
The torn PCL is removed, and tunnels are drilled into the femur (thigh bone) and tibia (shin bone) along the original ligament pathway.
A tendon graft is then passed through these tunnels to recreate the PCL.
The graft is fixed securely using screws, buttons, or other fixation devices.
In combined injuries (such as multi-ligament knee injuries), other structures (e.g., ACL, MCL, or posterolateral corner) may be reconstructed during the same procedure.
Surgery typically takes 90–120 minutes, and most patients stay overnight in hospital but can be sent home the day in certain clinical situation.
What Different Kinds of Grafts Are Used in PCL Reconstructions?
There are several graft options for PCL reconstructions, including hamstring/quadriceps from the patient and cadaver donor tissue (allograft). The decision as to which graft to use is based on other ligament injuries that require reconstruction, the morbidity of the graft that is being harvested, and the size/length of the graft. Currently, there is no sufficient evidence that one graft option has higher patient satisfaction or lower graft injury rate compared to others.
What Is the Recovery for PCL Reconstruction in the Immediate Postoperative Period?
Your post-operative recovery will be based on what other injuries are being treated (meniscus, ACL, MCL, etc) in addition to the PCL reconstruction. The typical rehabilitation for an isolated PCL reconstruction is as follows:
Hospital Stay: You will typically only require an overnight stay in hospital. There are situations where discharge home the same day of surgery can occur.
Weight bearing: You will be non-weight bearing for 8 weeks with the use of crutches. Afterward, you will gradually progress to full weight bearing at 10-12 weeks
Brace: You typically placed in a unique PCL brace, which pushed your tibia forward when bending your knee. Usually, the brace will be worn for 6-12 weeks to protect the graft.
Range of motion: Early motion starts right away with the PCL brace on.
Ice and elevation: Used frequently to control pain and swelling. An ice/compression machine can be hired from a 3rd party.
Physiotherapy: Starts a few days after surgery, focusing on gentle range-of-motion and quadriceps activation. Aggressive strengthening of the hamstrings starts at 8 weeks.
How is the Wound Managed?
It is normal for the top dressing to become moist with arthroscopic fluid in the first 1–2 days.
After 1-2 days, remove the outer dressing and leave the smaller waterproof dressings in place.
Dressings may be removed completely after 7 days.
Incisions typically heal within two weeks.
Showers are permitted while the wounds are covered with waterproof dressings during the first 2 weeks.
Do not submerge incisions in water (baths, pools, ocean) for 4 weeks.
A wound check with your GP at the two-week mark is recommended.
Absorbable sutures are typically used and do not require removal, though occasionally small remnants may naturally surface during healing.
How Do I Prevent Blood Clots (DVT/PE)?
Blood clots (deep vein thrombosis or pulmonary embolism) are uncommon but can occur after surgery.
You can reduce the risk by:
Moving your foot and ankle regularly while resting.
Walking early with assistance.
You will likely be instructed to take aspirin for 2-4 weeks to prevent DVT/PE.
Avoiding long periods of sitting or immobility.
Seek immediate medical attention if you develop calf pain, swelling, chest pain, or shortness of breath.
How Do I Manage My Pain After PCL Reconstruction?
Use ice regularly (20 minutes at a time, several times per day). You may hire an ice machine from a 3rd party.
Take prescribed pain relief medications as directed. Opioid medication can be used, but there are known side effects such as nausea, vomiting, constipation, and dependence; thus, non-opioid medications should be prioritized when medically tolerated.
Use a compressive dressing on the knee for 6-12 weeks to help with swelling
Begin gentle range-of-motion and muscle activation exercises as soon as recommended.
Use walking aids to help with gait
What Issues Should I Call the Clinic Regarding?
You should contact your surgeon or clinic immediately if you notice:
Increasing redness, swelling, or foul-smelling drainage from the wound.
Persistent or worsening pain not controlled by medication.
Fever, chills, or night sweats.
Calf pain or swelling (possible blood clot).
Acute injury to your operative extremity.
Prompt review allows early management of potential complications.
When Can I Return to Normal Activities or Sports After PCL Reconstruction?
PCL reconstruction requires a longer recovery than most other ligament procedures.
Return to activities depends on the nature and intensity of the recreation
This is a general guideline:
Running: once knee swelling, pain have resolved, and adequate strength has been retained- typically 4-5 months
Non-cutting activities/sport (golf, cricket, surfing, etc), typically 7-9 months
Training for sport, typically 9-12 months
Cutting sports (football, rugby, basketball, netball, etc), typically 12-18 months
There are no strict guidelines on when to return to sport after revision PCL reconstruction but it typically takes 12-18 months.
When Can I Drive?
You can usually drive when you can safely control the vehicle and perform an emergency stop comfortably.
This is typically around 4–6 weeks after surgery for right knee surgery, and 2-3 weeks for the left knee.
You must not drive while taking strong pain medication (e.g., opioids).
When Can I Return to Work?
Return to work depends on your occupation:
Office or sedentary work: 1–2 weeks (once you can safely commute).
Light manual work: 4–6 weeks.
Heavy manual labour: 3–4 months or longer, depending on recovery.
Should I See a Physiotherapist?
Yes. Physiotherapy is essential for optimal recovery and long-term success after ACL reconstruction.
Your physiotherapist will:
Guide you through a structured rehabilitation program.
Focus on restoring range of motion, strength, balance, and neuromuscular control.
Progress exercises gradually from early mobility to return-to-sport conditioning.
Most patients continue physiotherapy for 6–12 months to achieve full recovery, including returning to sport.
What Are the Complications After an ACL Reconstruction?
While PCL reconstruction is a safe and effective procedure, potential complications include:
Infection (rare)
Blood clots (DVT/PE)
Neurovascular injury/ Compartment syndrome: The popliteal artery is very close to the tunnels drilled in the knee. While not common, the risk of injury to this artery can occur, which is limb-threatening.
Knee stiffness or limited range of motion
Persistent posterior laxity or instability (very common even after well-performed PCL reconstruction)
Graft re-rupture or failure
Hardware irritation (occasionally requires removal)
Numbness or tingling around the incision site
Donor site soreness or weakness (if the patient’s own tissue graft is used)
Chronic swelling or discomfort with kneeling or deep flexion
Progression of knee arthritis
Failure of repair or reconstruction of other injuries in the knee