Anterior Cruciate Ligament (ACL) Reconstruction
How Is An ACL Reconstruction Performed?
An ACL reconstruction is performed to restore stability to the knee after a torn anterior cruciate ligament. The procedure is done arthroscopically (keyhole surgery) under general anesthesia.
During the operation:
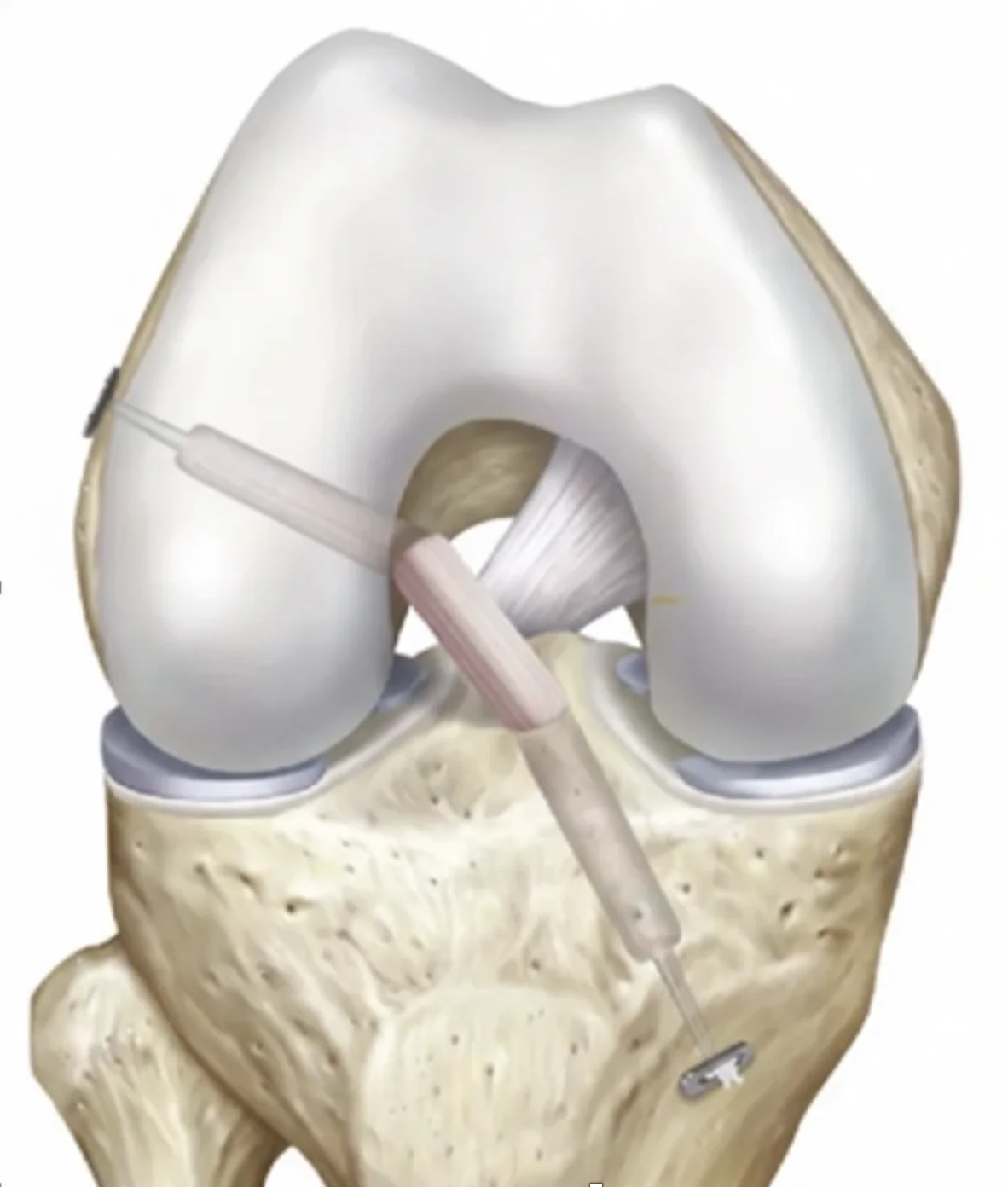
Small incisions are made to insert a camera and instruments into the knee.
The torn ACL is removed, and tunnels are drilled in the femur (thigh bone) and tibia (shin bone) where the new graft will be placed.
A tendon graft is passed through these tunnels to recreate the ligament’s normal path.
The graft is fixed with screws or buttons to hold it securely while it heals into the bone.
If indicated, additional procedures (e.g., meniscus repair or lateral extra-articular tenodesis) are performed at the same time.
The procedure usually takes 60–90 minutes, and most patients go home the same day or the following morning.
What Different Kinds Of Grafts Are Used?
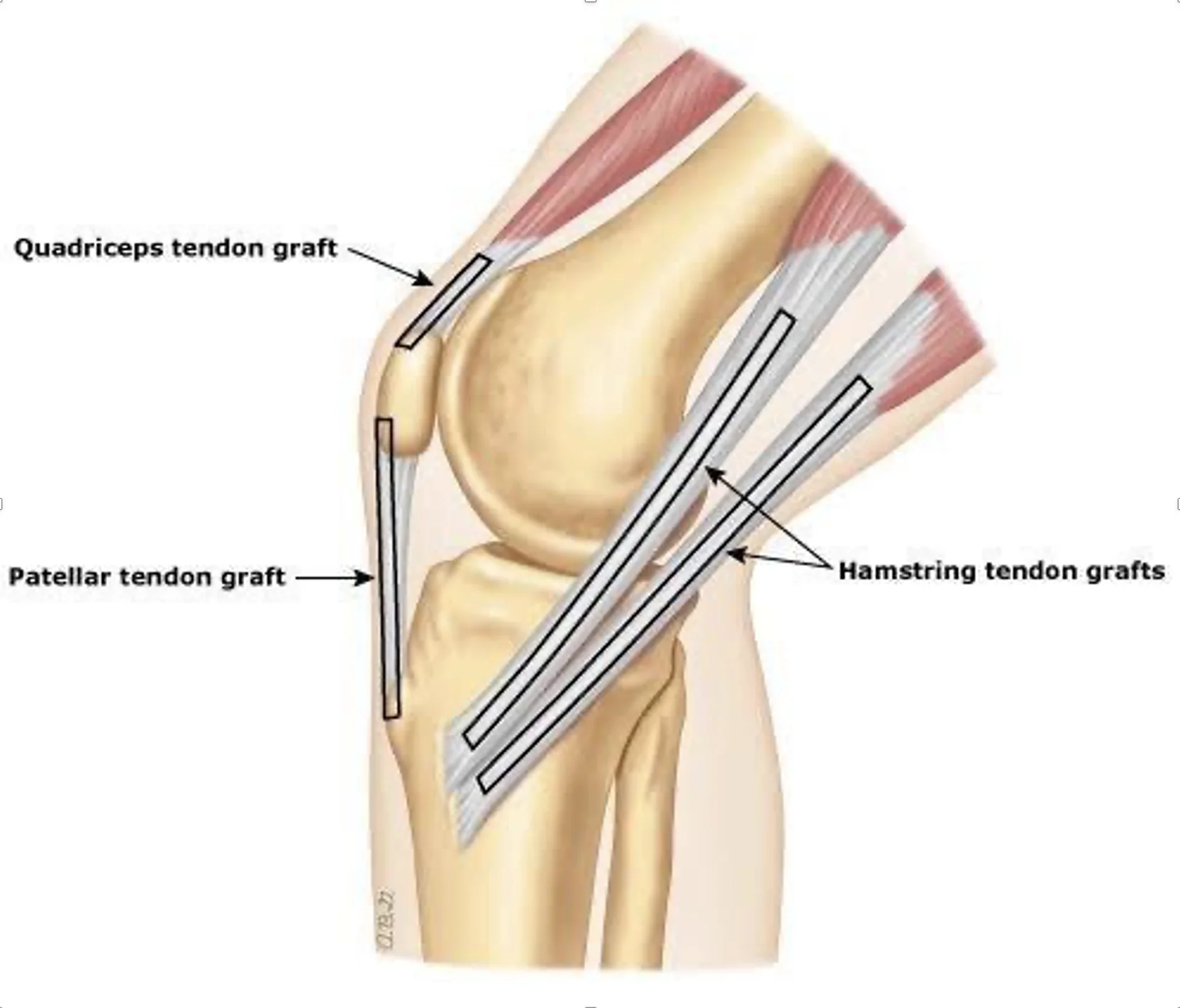
There are several graft options for ACL reconstruction. The choice depends on age, activity level, and surgeon preference.
Hamstring Tendon Autograft
This is sourced from your own gracilis and semitendinosus tendons.
Advantages: Small incision, less anterior knee pain, easier to rehab quadriceps.
Disadvantages: Loss of hamstring strength, higher graft rupture rate.
Patellar Tendon Autograft (BTB)
This is sourced from the middle third of patellar tendon with bone plugs.
Advantages: Lowest graft rupture rate. Very stiff graft.
Disadvantages: More anterior knee pain, longer recovery from kneeling, weakness in quadriceps, increased risk of contralateral ACL tear.
Quadriceps Tendon Autograft
This is sourced from a partial thickness quadriceps tendon.
Advantages: Large, strong graft; low donor site pain.
Disadvantages: Quadriceps weakness, unknown graft failure rate compared to other grafts.
Allograft (Donor Tissue)
This is sourced from a cadaver tissue bank.
Advantages: No donor site pain, easier post-operative rehabilitation.
Disadvantages: Higher graft failure rate in younger/active patients.
What Are The Advantages And Disadvantages Of A Lateral Extra-Articular Tenodesis (LEAT)?
A Lateral Extra-Articular Tenodesis (LEAT) is sometimes performed in addition to ACL reconstruction to improve rotational control and reduce the risk of graft re-tear.
Advantages:
Provides additional rotational stability to the knee.
Reduces the risk of re-injury, especially in high-demand or pivoting sports.
Useful in revision ACL surgery or in patients with generalised laxity.
Disadvantages:
Increases discomfort after surgery, which slows early rehab.
May cause a defect on the outer aspect of the knee
Risk of over-constraining the knee, unknown if this increases the risk of arthritis
How Is a LEAT Performed?
A LEAT is performed through an incision on the outer (lateral) side of the knee.
A strip of the iliotibial (IT) band is taken and passed under the LCL and either secured to the femur or tibia based on how it was harvested. This provides extra-rotational stability to the knee after ACL reconstruction.
This procedure is completed during the same operation as the ACL reconstruction.
What Is the Recovery for an ACL Reconstruction in the Immediate Postoperative Period?
Hospital stay: You will typically be admitted to hospital for one night, but there are situations where you can be sent home the day of surgery.
Weight bearing: You will usually begin walking with crutches immediately after surgery. Some forms of meniscus repairs may restrict your weight-bearing for 6 weeks.
Brace: A knee brace is not normally used after ACL reconstructions. A brace will only be used to protect some types of meniscus repairs that occur during the same procedure.
Ice and elevation: Regular icing and leg elevation reduce swelling and pain. A compression ice machine can be hired from a 3rd party.
Physiotherapy: Early exercises begin within days to restore knee motion and prevent stiffness, especially regaining full extension. You should start riding a stationary bike right away after surgery.
How is the Wound Managed?
It is normal for the top dressing to become moist with arthroscopic fluid in the first 1–2 days.
After 1-2 days, remove the outer dressing and leave the smaller waterproof dressings in place.
Dressings may be removed completely after 10-14 days.
Incisions typically heal within two weeks.
Showers are permitted while the wounds are covered with waterproof dressings during the first 2 weeks.
Do not submerge incisions in water (baths, pools, ocean) for 4 weeks.
A wound check in our clinic, your GP, or allied health professional at the two-week mark is recommended.
Absorbable sutures are typically used and do not require removal, though occasionally small remnants may naturally surface during healing.
How Do I Prevent Blood Clots (DVT/PE)?
Blood clots (deep vein thrombosis or pulmonary embolism) can occur after surgery.
You can reduce the risk by:
Moving your foot and ankle regularly while resting.
Walking early with assistance.
You will likely be instructed to take aspirin for 2-4 weeks to prevent DVT/PE.
Avoiding long periods of sitting or immobility.
Seek immediate medical attention if you develop calf pain, swelling, chest pain, or shortness of breath.
How Do I Manage My Pain After ACL Reconstruction?
Use ice regularly (20 minutes at a time, several times per day). You may hire an ice machine from a 3rd party.
Take prescribed pain relief medications as directed. Opioid medication can be used but they cause nausea, vomiting, constipation, and dependance; thus, non-opioid medications should be prioritized when medically tolerated.
Use a compressive dressing on the knee for 6-12 weeks to help with swelling
Begin gentle range-of-motion and muscle activation exercises as soon as recommended.
Use walking aids to help with walking
What Issues Should I Call The Clinic Regarding?
You should contact your surgeon or clinic immediately if you notice:
Increasing redness, swelling, or foul-smelling drainage from the wound.
Persistent or worsening pain not controlled by medication.
Fever, chills, or night sweats.
Calf pain or swelling (possible blood clot).
Acute injury to your operative extremity.
Prompt review allows early management of potential complications.
When Can I Drive?
You can usually drive when you can safely control the vehicle and perform an emergency stop comfortably.
This is typically around 4–6 weeks after surgery for right knee surgery, and 2-3 weeks for the left knee.
You must not drive while taking strong pain medication (e.g., opioids).
When Can I Return To Work?
Return to work depends on your occupation:
Office or sedentary work: 1–2 weeks (once you can safely commute).
Light manual work: 4–6 weeks.
Heavy manual labour: 3–4 months or longer, depending on recovery.
Should I See A Physiotherapist?
Yes. Physiotherapy is essential for optimal recovery and long-term success after ACL reconstruction.
Your physiotherapist will:
Guide you through a structured rehabilitation program.
Focus on restoring range of motion, strength, balance, and neuromuscular control.
Progress exercises gradually from early mobility to return-to-sport conditioning.
Most patients continue physiotherapy for 6–12 months to achieve full recovery, including returning to sport.
What Are The Complications After An ACL Reconstruction?
While ACL reconstruction is highly successful, all surgeries carry risks.
Possible complications include:
Infection (rare)
Blood clots (DVT/PE)
Knee stiffness or loss of motion
Persistent swelling or pain
Numbness around incision sites
Graft failure or re-rupture (particularly if returning to sport too early)
Hardware irritation
Donor site pain
Residual instability
Progression of arthritis
Failure of meniscus repair
Weakness of thigh musculature
Inability to return to sport
When Can I Return To Activities And Sports?
Return to activities depends on the nature and intensity of the recreation
This is a general guideline:
Running: once knee swelling and pain have resolved, typically 3-4 months
Non-cutting activities/sport (golf, cricket, surfing, etc), typically 6-9 months
Training for sport, typically 6-9 months
Cutting sports (football, rugby, basketball, netball, etc), typically 9-12 months
Returning to sports before 9 months increases your risk of ACL graft tears. Unfortunately, not all patients will be able to return to their previous activities/sports.