Revision Anterior Cruciate Ligament (ACL) Reconstruction
Why Do ACL Reconstructions Fail?
ACL reconstructions can fail for several reasons, often related to technical, biological, or patient-specific factors. Common causes include:
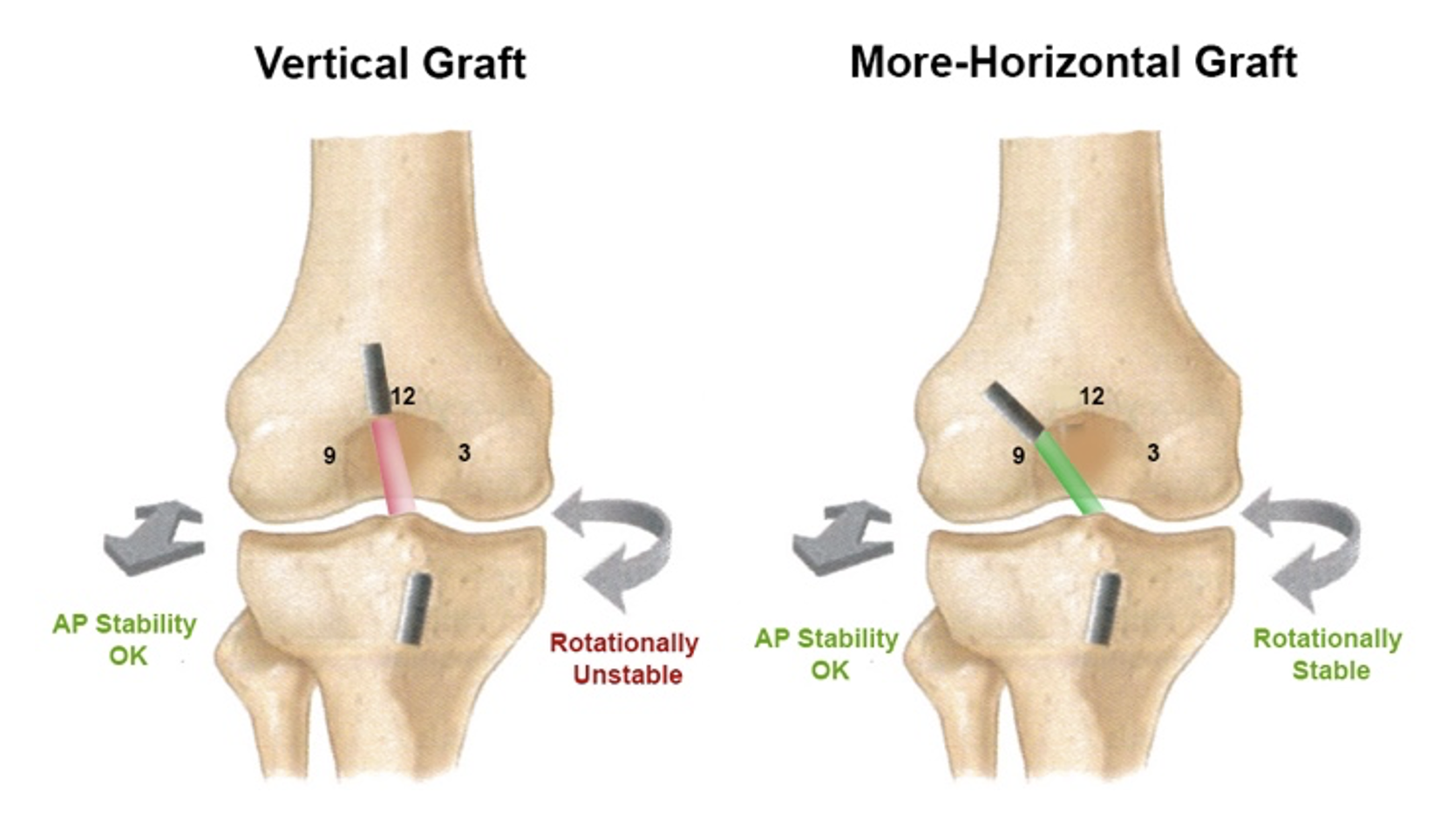
Technical errors – Incorrect tunnel placement (too vertical or too anterior) is the most common cause, leading to persistent instability or graft impingement.
Traumatic re-injury – A new accident or pivoting event that exceeds graft strength.
Biological factors – Due to poor integration of the graft after surgery, leading to stretching or rupture over time.
Missed or untreated associated injuries – Damage to structures such as the meniscus, posterolateral corner, or MCL can cause residual instability.
Infection – Though rare, it can weaken or destroy the graft.
Early return to sport – Returning to pivoting or contact sports before full graft maturation (typically <9 months) increases re-tear risk.
Poor rehabilitation – Inadequate physiotherapy or muscle imbalance can compromise knee stability and control.
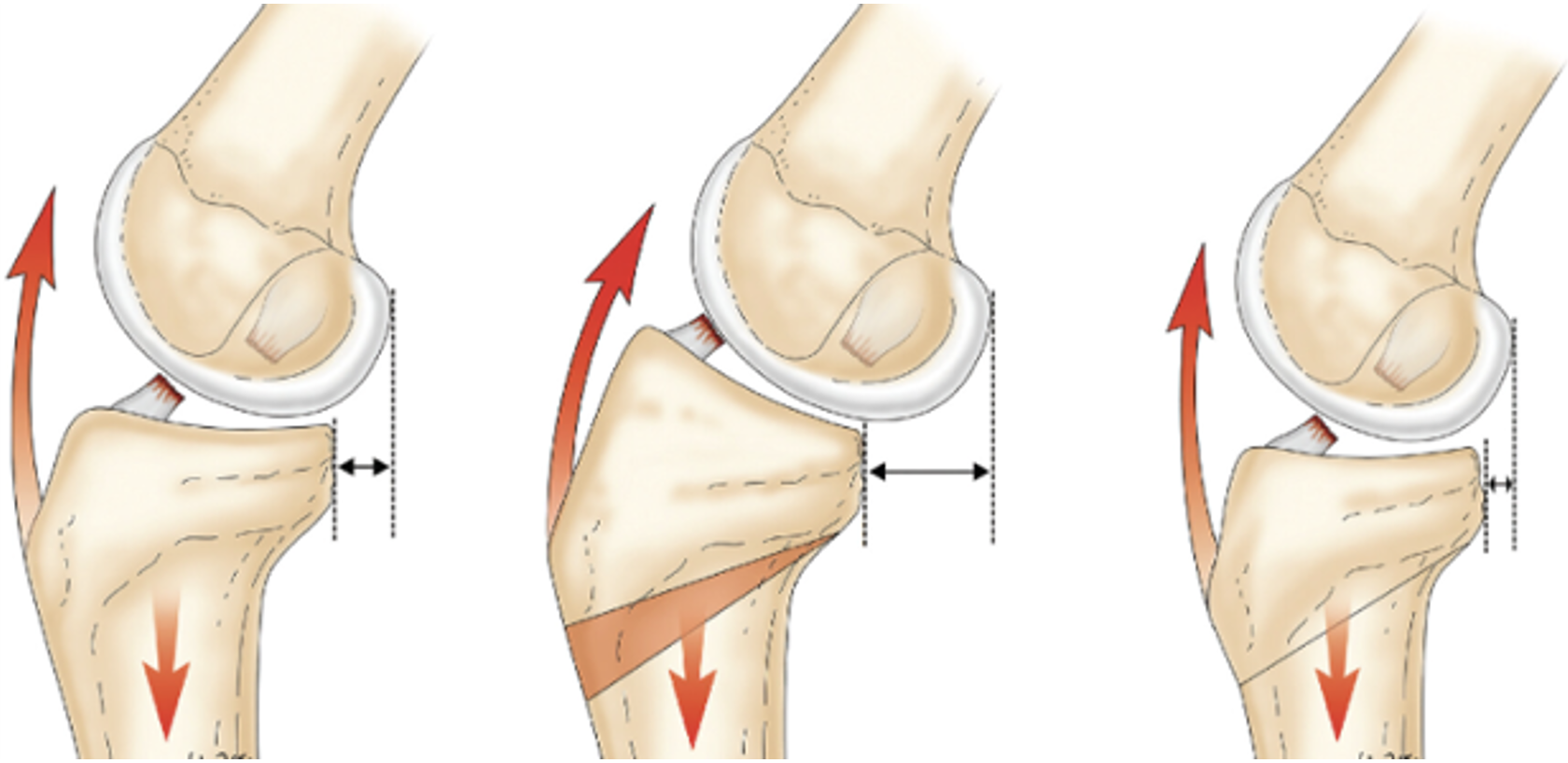
Bone architecture – Poor limb alignment or architecture (such as increased tibial slope) can increase the forces experienced by the ACL graft, causing it to rupture during activities.
Revision surgery aims to address these underlying issues to restore long-term stability.
How Is a Revision ACL Reconstruction Performed?
A revision ACL reconstruction is performed when a previous ACL graft has failed — either by stretching, rupturing, or not restoring full knee stability.
Because the knee has already been operated on, revision surgery is more technically demanding and carefully planned using MRI and CT scans to evaluate existing tunnels, hardware, and bone quality.
During surgery:
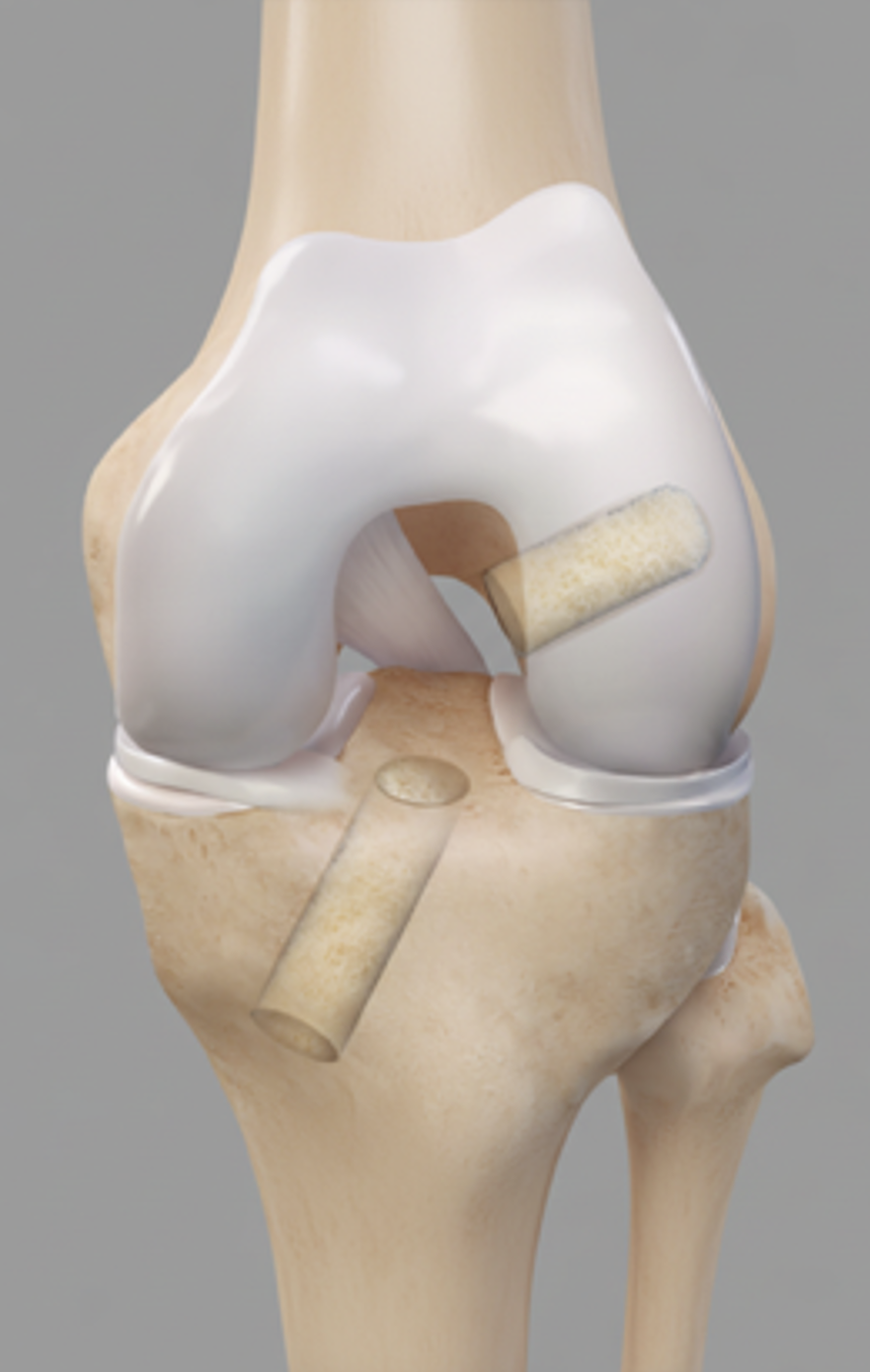
Previous hardware is assessed and removed if necessary.
The previous bone tunnels are evaluated — if they are well-positioned, they may be reused; if mispositioned or widened, the previous tunnels may need to be bone grafted.
In some cases, a staged procedure is required, where the tunnels are bone grafted and allowed to heal before definitive reconstruction.
A new graft is passed through the bone tunnels and fixed securely with screws or buttons.
A lateral extra-articular tenodesis (LEAT) may be added to improve rotational control and reduce the risk of re-rupture.
Other ligament injuries (such as a posterior lateral corner injury) that could have been missed during the primary procedure may be reconstructed
Osteotomies (bone realignment) may need to be performed if the extremity has poor alignment or bone architecture that increases the risk of graft failure
Previously missed meniscus injuries may need to be repaired. Rarely, some cases of deficient menisci require a transplant from a cadaver donor.
A new graft will have to be harvested either from the same extremity or even from the opposite knee.
What Are the Advantages and Disadvantages of Adding a Lateral Extra-Articular Tenodesis (LEAT)?
Advantages:
Adds extra rotational control to the knee.
Improves pivot-shift stability and confidence during cutting movements.
Some evidence displays that adding a LEAT can reduce revision graft rupture rates, but this evidence is controversial.
Disadvantages:
Slightly slower early recovery and increased postoperative pain
Rare risk of over-constraint, which may potentially worsen the risk of knee arthritis.
Requires an additional incision.
LEAT is often recommended in revision ACL reconstructions because it improves graft protection and rotational stability.
What Is the Recovery in the Immediate Postoperative Period?
Hospital stay: You will typically be admitted to hospital for one night, but there are situations where you can be sent home the day of surgery.
Weight bearing: You will usually begin walking with crutches immediately after surgery. Some forms of meniscus repairs may restrict your weight-bearing for 6 weeks.
Brace: A knee brace is not normally used after revision ACL reconstructions. A brace will only be used to protect some types of meniscus repairs that occur during the same procedure.
Ice and elevation: Regular icing and leg elevation reduce swelling and pain. A compression ice machine can be hired from a 3rd party.
Physiotherapy: Early exercises begin within days to restore knee motion and prevent stiffness. You should start riding a stationary bike right away after surgery.
How Is the Wound Managed?
It is normal for the top dressing to become moist with arthroscopic fluid in the first 1–2 days.
After 1-2 days, remove the outer dressing and leave the smaller waterproof dressings in place.
Dressings may be removed completely after 7 days.
Incisions typically heal within two weeks.
Showers are permitted while the wounds are covered with waterproof dressings during the first 2 weeks.
Do not submerge incisions in water (baths, pools, ocean) for 4 weeks.
A wound check with your GP at the two-week mark is recommended.
Absorbable sutures are typically used and do not require removal, though occasionally small remnants may naturally surface during healing.
How Do I Prevent Blood Clots (DVT/PE)?
Blood clots (deep vein thrombosis or pulmonary embolism) are uncommon but can occur after surgery.
You can reduce the risk by:
Moving your foot and ankle regularly while resting.
Walking early with assistance.
You will likely be instructed to take aspirin for 2-4 weeks to prevent DVT/PE.
Avoiding long periods of sitting or immobility.
Seek immediate medical attention if you develop calf pain, swelling, chest pain, or shortness of breath.
How Do I Manage My Pain After Revision ACL Reconstruction?
Use ice regularly (20 minutes at a time, several times per day). You may hire an ice machine from a 3rd party.
Take prescribed pain relief medications as directed. Opioid medication can be used, but they cause nausea, vomiting, constipation, and dependence; thus, non-opioid medications should be prioritized when medically tolerated.
Use a compressive dressing on the knee for 6-12 weeks to help with swelling
Begin gentle range-of-motion and muscle activation exercises as soon as recommended.
Use walking aids to help with gait
What Issues Should I Call the Clinic Regarding?
You should contact your surgeon or clinic immediately if you notice:
Increasing redness, swelling, or foul-smelling drainage from the wound.
Persistent or worsening pain not controlled by medication.
Fever, chills, or night sweats.
Calf pain or swelling (possible blood clot).
Acute injury to your operative extremity.
Prompt review allows early management of potential complications.
When Can I Return to Normal Activities or Sports After Revision ACL Reconstruction?
Return to activities depends on the nature and intensity of the recreation
This is a general guideline:
Running: once knee swelling and pain have resolved, typically 3-4 months
Non-cutting activities/sport (golf, cricket, surfing, etc), typically 6-9 months
Training for sport, typically 6-12 months
Cutting sports (football, rugby, basketball, netball, etc), typically 12-18 months
There are no strict guidelines on when to return to sport after revision ACL reconstruction but it typically takes 12-18 months.
When Can I Drive?
You can usually drive when you can safely control the vehicle and perform an emergency stop comfortably.
This is typically around 4–6 weeks after surgery for right knee surgery, and 2-3 weeks for the left knee.
You must not drive while taking strong pain medication (e.g., opioids).
When Can I Return to Work?
Return to work depends on your occupation:
Office or sedentary work: 1–2 weeks (once you can safely commute).
Light manual work: 4–6 weeks.
Heavy manual labour: 3–4 months or longer, depending on recovery.
Should I See a Physiotherapist?
Yes. Physiotherapy is essential for optimal recovery and long-term success after ACL reconstruction.
Your physiotherapist will:
Guide you through a structured rehabilitation program.
Focus on restoring range of motion, strength, balance, and neuromuscular control.
Progress exercises gradually from early mobility to return-to-sport conditioning.
Most patients continue physiotherapy for 6–12 months to achieve full recovery, including returning to sport.
What Are the Complications After a Revision ACL Reconstruction?
Revision ACL reconstructions have a higher complication rate compared to primary ACL reconstructions.
Possible complications include:
Infection (rare)
Blood clots (DVT/PE)
Knee stiffness or loss of motion
Persistent swelling or pain
Numbness around incision sites
Graft failure or re-rupture (increased risk in revision ACL reconstructions compared to primary surgery)
Hardware irritation
Donor site pain
Residual instability
Progression of arthritis
Failure of meniscus repair
Weakness of thigh musculature
Inability to return to sport
Failure of associated ligament injury repairs/reconstructions
Osteotomy/bone graft nonunion