Patella Stabilisation
What procedures are performed when stabilising a Patella?
Patella stabilisation procedures are performed to prevent the kneecap (patella) from dislocating or sliding out of its normal position in the groove at the front of the femur. Patellar instability can occur due to injury, ligament laxity, or abnormal anatomy such as a shallow trochlear groove or high-riding patella.
Common procedures include:
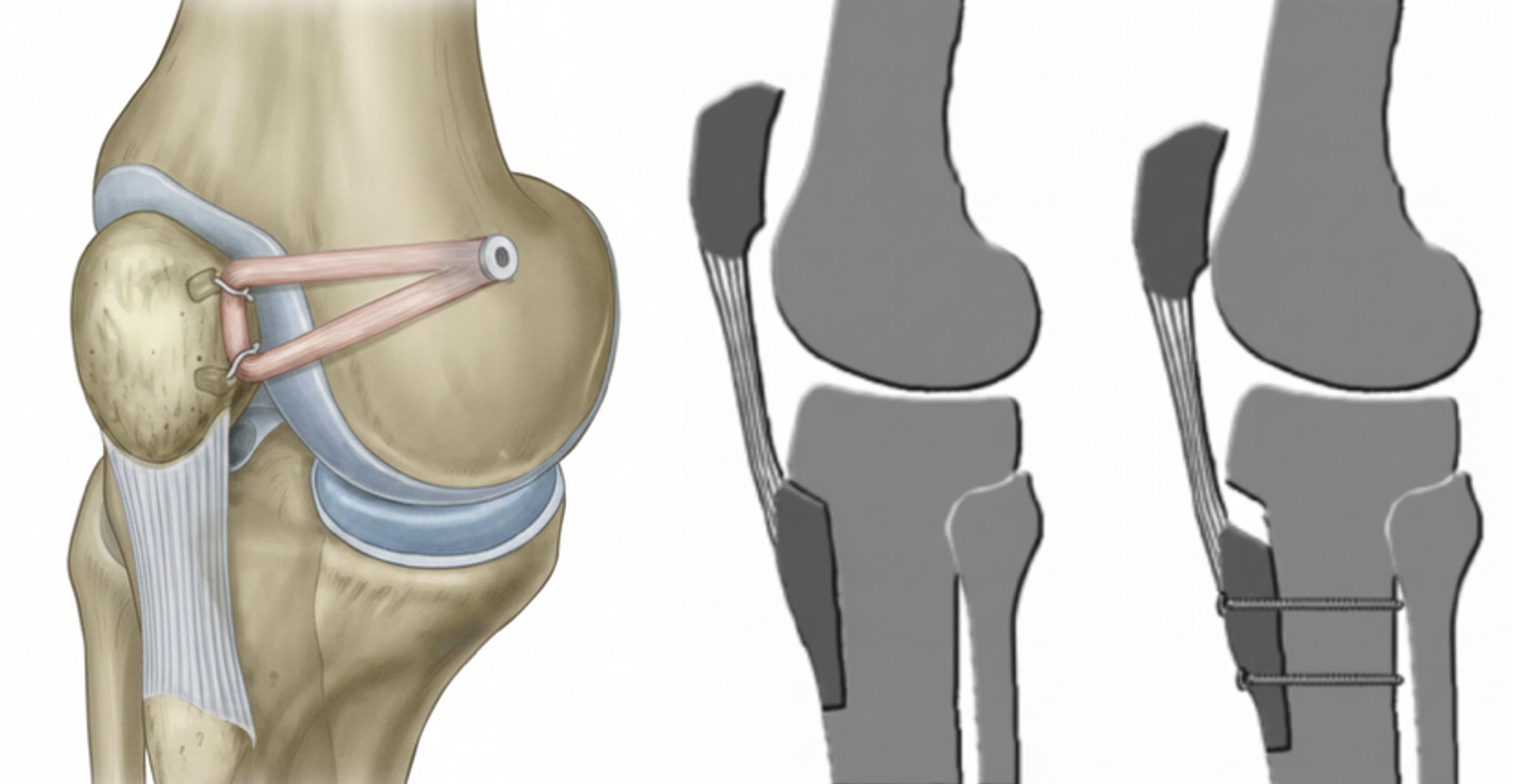
Medial Patellofemoral Ligament (MPFL) Reconstruction – the most common procedure, where a new ligament is created using a tendon graft to replace the torn MPFL that stabilizes the patella on the inner side of the knee.
Tibial Tubercle Osteotomy (TTO) – involves shifting the bony attachment of the patellar tendon to realign the patella and improve tracking.
Trochleoplasty – reshaping the groove on the femur (trochlea) when it is too shallow or flat.
Femoral/tibial osteotomy – occasionally performed to align the knee to improve patella tracking
Fixing or removal of osteochondral fragments
The specific combination of procedures depends on the underlying cause of instability and your individual anatomy.
What Is the Recovery in the Immediate Postoperative Period?
Hospital stay: Most patients stay 1-2 days in hospital working with physiotherapy.
Weight bearing: You will walk on the operated leg immediately with gait aids.
Brace: You will likely require a brace to be worn for 6 weeks
Range of motion: Early passive range of motion will start right after surgery. The specific progression of restrictions depends on the procedures that are performed to stabilize the patella.
Ice and elevation: Used frequently to control pain and swelling. You should ice for 20 minutes, 3–4 times per day right after surgery. An ice/compression machine can be hired from a third party.
Assistive devices: You may use a walker or crutches for 6 weeks after surgery, progressing to a cane as comfort improves. It can take up to 6–12 weeks before you can walk independently.
How Is the Wound Managed?
Bulky dressings will be removed 1–2 days after surgery.
A waterproof underlay dressing should be left on for 2 weeks.
Incisions typically heal within 2 weeks.
Showers are permitted while wounds are covered with waterproof dressings during the first 2 weeks.
Do not submerge incisions in water (baths, pools, or ocean) for 6 weeks.
A wound check with your GP, allied health provider, or our clinic is recommended at 2 weeks.
Absorbable sutures are usually used and do not require removal, though small remnants may surface naturally during healing.
How Do I Prevent Blood Clots (DVT/PE)?
Blood clots (deep vein thrombosis or pulmonary embolism) can occur after surgery.
You can reduce the risk by:
Moving your foot and ankle regularly while resting.
Walking early with assistance.
Avoiding long periods of sitting or immobility.
Wearing compression stockings for the first 4–6 weeks.
You will likely take aspirin for 2–6 weeks to prevent DVT/PE. If you have a history of blood clots or risk factors, a stronger blood thinner may be prescribed.
If you plan any long-distance travel within 6 weeks of surgery, please inform our clinic for preventative medication.
Seek immediate medical attention if you develop calf pain, swelling, chest pain, or shortness of breath.
How Do I manage my pain after a Patella Stabilisation procedure?
Your anaesthetist will discuss possible spinal or regional nerve blocks to help control pain immediately after surgery.
Local anaesthetic will be injected into the knee during surgery.
Use ice regularly (20 minutes, 3–4 times per day). An ice machine may be hired from a third party.
Take prescribed pain medication as directed. Opioids may be used short-term but have known side effects (nausea, constipation, dependence). Non-opioid medications are preferred when tolerated.
Use a compression dressing on the knee for 6–12 weeks to manage swelling.
Begin gentle range-of-motion and muscle activation exercises as soon as recommended.
Use walking aids for stability while recovering your gait.
What Issues Should I Call the Clinic Regarding?
You should contact your surgeon or clinic immediately if you notice:
Increasing redness, swelling, or drainage from the wound.
Persistent or worsening pain not controlled by medication.
Fever, chills, or night sweats.
Calf pain or swelling (possible blood clot).
Any acute injury to your operative knee.
Prompt review allows early management of potential complications.
When Can I Return to Normal Activities After Patella Stabilization?
Return to activities depends on the nature and intensity of the activity and the procedures that were performed. Typically, running will take 4-5 months. Return to sports can take 6-12 months.
When Can I Drive?
You can usually drive once you can safely control the vehicle and perform an emergency stop comfortably.
This is typically 8–10 weeks after right knee surgery, and 2–3 weeks for the left knee.
You must not drive while taking strong pain medication (e.g., opioids).
When Can I Return to Work?
Return to work depends on your occupation and the type of surgery you received. In general, the following time are followed:
Office or sedentary work: 1–2 weeks (once you can commute safely).
Light manual work: 4–6 weeks.
Heavy manual labour: 3–4 months or longer, depending on recovery.
Should I See a Physiotherapist?
Yes. Physiotherapy is essential for optimal recovery and long-term success after patella stabilization.
Your physiotherapist will:
Guide you through a structured rehabilitation program.
Focus on restoring range of motion, strength, balance, and gait mechanics.
Progress exercises gradually from early mobility to functional activity and low-impact sport.
Most patients continue physiotherapy for 6–12 months to achieve full functional recovery.
What Are the Complications After a Patella Stabilization Procedure?
While patella stabilization is a safe and effective procedure, all surgeries carry potential risks.
Possible complications include:
Infection (superficial or deep)
Blood clots (DVT/PE)
Knee stiffness or limited range of motion
Persistent pain or swelling
Graft failure or recurrent instability
Numbness around the incision site
Fracture of the patella or tibial tubercle (rare)
Hardware irritation (may require removal)
Nonunion of osteotomy
Overcorrection of osteotomies (creating knee stiffness or progressive arthritis)
Progressive patellofemoral arthritis
Difficulty kneeling
Unable to return to previous activities and/or sport